Forgotten Vitamin MK7
Vitamin K naturally exists in two forms, vitamin K1 (phylloquinone) and a series of Vitamin K2 (menaquinones). Menaquinones (MKs) are so different from phylloquinone and represent a family of compounds with isoprenoid side chains of varying lengths. These side chains consist of 4 to 13 isoprenyl units named MK-4 to MK-13. The major dietary source of phylloquinone are green vegetables, whereas menaquinones are primarily of microbial origin and are present in certain animal products and fermented foods.
Biologically, MK7 is the superior form for supplementation that helps with inhibition of cartilage calcification, reducing the chronic inflammation and promoting bone density by binding calcium to the bone matrix just to name a few. Other MK forms do not deliver equal benefits and their presence is fundamentally undesirable.
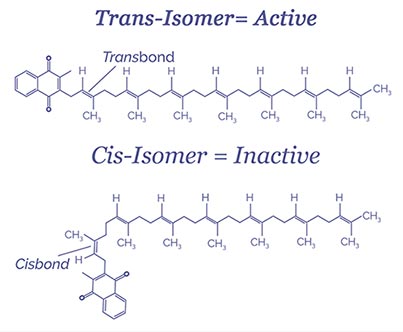
Many people have not yet realized that MK7 can exist as cis and trans isomers. The chemical structure of MK7 influences its ability to interact with subcellular structures, and thus determines its biological activity. MK7 cis-isomers have a bend in their carbon chain and are not active. Only trans-isomer MK7 are considered to be bioactive. Many K2 ingredients have a mixture of cis and trans isomers, depending on how well they are produced. You’ll want to look for K2 supplements with a high percentage of trans-isomer MK7, ideally 100%. In finished capsules and tablets, however, the current USP MK7 monograph does not require cis vs. trans determination. This opens a door in markets for low quality MK7 ingredient that does not deliver value, and brands and consumers ultimately pay the price for this. Consumer product testing studies repeated over several years consistently demonstrate unacceptably high numbers of biologically inactive cis MK7 products sold to consumers.
MK7 puts calcium into balance
Calcium is an essential nutrient and the body’s most abundant mineral. Calcium is vital for bone health, is the primary component of the bone matrix, and protects against bone diseases like osteoporosis. Calcium helps regulate muscle contraction, nerve signalling and other critical functions. Calcium is among the top-selling ingredients for supplementation and food fortification and awareness and usage among consumers is high.
However, the soft tissues of the body, especially the cartilage and vessels of the circulatory system, can begin to absorb and integrate calcium in an unhealthy process called tissue calcification. Skin callouses and kidney stones are other examples of tissue calcification or improper utilization of calcium by the body.
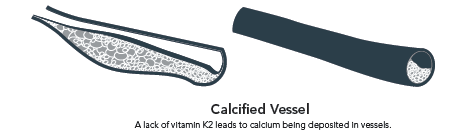
MK7 provides dual-action regulation of calcium in the body. This regulation helps maintain calcium balance and good health. K2 is the necessary co-factor for the activation of osteocalcin proteins that are produced by osteoblast cells in bones. Activated osteocalcin binds with free-floating calcium in the blood and transports them to the bone matrix. Moreover, Gla-Rich and Matrix Gla proteins which inhibit cartilage calcification are also MK7 dependent and the absence of this vitamin impairs capacity of decalcification. Therefore, MK7 plays a crucial role in preventing cartilage calcification and stiffening.
To summarise the trans form of MK7 helps with:
1) inhibiting cartilage calcification,
2) reducing the chronic inflammation, and
3) promoting bone density by binding calcium to the bone matrix.
Did you know MK7 Can help with Reversing Calcification?
Several studies have shown a strongest evidence that MK7 supplementation can reverse existing levels of calcification and restore soft tissues flexibility.
“Calcium can accumulate in soft tissues causing them to harden and become less flexible“
MK7 deficiency
MK7 deficiency is common in Western populations. Fermented food products like fermented soybeans with Bacillus subtilis var. natto are the primary sources of MK7.

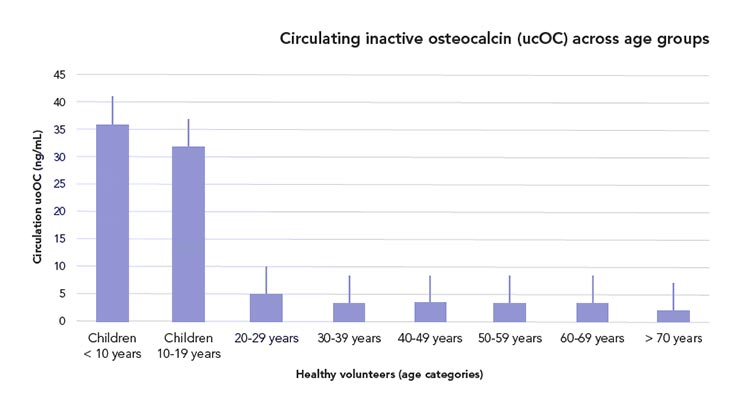
In Western populations, the daily intake of MK7 via food has decreased over the past hundred years. The statuses of carboxylated and uncarboxylated osteocalcin and MGP in the blood are important biomarkers for measuring the MK7 status in the human body.
MK7 and athletic performance
An influential 2015 study showed that MK7 supplementation over three years improved and restored arterial flexibility compared to controls. More recently, a study among athletes by McFarlin et al. demonstrated a 12% increase in maximal cardiac output after just 8 weeks of oral MK7 supplementation. The study addressed the effect of vitamin K2 on heart muscle function during maximal aerobic exercise in active individuals. The authors report that to achieve similar increases in maximal cardiac output (without K2 supplementation) athletes would require 6-9 months of continuous training. K2 supplementation may reduce required training periods by 60%. This study investigated K2 effects on the production of mitochondrial adenosine triphosphate (ATP), which represents study of an entirely new K2 mechanism of action on heart performance, and muscles in general.
MK7 and Inflammation
MK7 has been shown to fight inflammation by inhibiting pro-inflammatory markers produced by white blood cells called monocytes. Researchers looking at the effect of MK7 on rheumatoid arthritis (an autoimmune inflammatory condition that affects the entire body but particularly the joints) found that Supplementation with MK7 lowered levels of inflammatory markers.
MK7 and Blood sugar balance
MK7 helps to activate and build-up stores of carboxylated osteocalcin in the bone. When needed, this supply of osteocalcin is regularly decarboxylated and released into the bloodstream, where it is used by the pancreas to increase insulin production, and by the rest of the body to improve insulin sensitivity and glucose metabolism. Studies show that mice who lack the osteocalcin producing gene suffer from poor glucose tolerance, insulin levels and insulin sensitivity. Pre-diabetics and untreated diabetics have decreased levels of serum osteocalcin.
Take home messages
- Vitamin K2 (MK7) helps to maintain flexible joints.
- Vitamin K2 (MK7) activates a protein that directs calcium away from cartilage and other soft tissues.
- Vitamin K2 (MK7) helps to maintain a healthy heart and blood circulatory system.
- Vitamin K2 (MK7) helps to maintain a healthy bone.
- Vitamin K2 (MK7) helps trained athletes maintain maximal cardiac output during aerobic exercise.
References
- M. Y. Speer, H.-Y. Yang, T. Brabb, E. Leaf, A. Look, W.-L. Lin, A. Frutkin, D. Dichek, and C. M. Giachelli, “Smooth Muscle Cells Give Rise to Osteochondrogenic Precursors and Chondrocytes in Calcifying Arteries,” Circulation Research, vol. 104, no. 6, pp. 733–741, May 2009.
- Kurnatowska, P. Grzelak, A. Masajtis-Zagajewska, M. Kaczmarska, L. Stefańczyk, C. Vermeer, K. Maresz, and M. Nowicki, “Effect of vitamin K2 on progression of atherosclerosis and vascular calcification in nondialyzed patients with chronic kidney disease stages 3–5,” Polish Archives of Internal Medicine, vol. 125, no. 9, pp. 631–640, 2015.
- M. H. J. Knapen, Lavienja A. J. L. M. Braam, N. E. Drummen, O. Bekers, A. P. G. Hoeks, and C. Vermeer, “Menaquinone-7 supplementation improves arterial stiffness in healthy postmenopausal women,” Thrombosis and Haemostasis, vol. 113, no. 05, pp. 1135–1144, 2015.
- M. J. H. V. Summeren, Lavienja A. J. L. M. Braam, M. R. Lilien, L. J. Schurgers, W. Kuis, and C. Vermeer, “The effect of menaquinone-7 (vitamin K2) supplementation on osteocalcin carboxylation in healthy prepubertal children,” British Journal of Nutrition, vol. 102, no. 08, p. 1171, 2009.
- K. Motohara, S. Takagi, F. Endo, Y. Kiyota, and I. Matsuda, “Oral Supplementation of Vitamin K for Pregnant Women and Effects on Levels of Plasma Vitamin K and PIVKA-II in the Neonate,” Journal of Pediatric Gastroenterology and Nutrition, vol. 11, no. 1, pp. 32–36, 1990.
- H. Katsuyama, S. Ideguchi, M. Fukunaga, K. Saijoh, and S. Sunami, “Usual Dietary Intake of Fermented Soybeans (Natto) Is Associated with Bone Mineral Density in Premenopausal Women.,” Journal of Nutritional Science and Vitaminology, vol. 48, no. 3, pp. 207–215, 2002.
- M. Møller, I. M. F. Gjelstad, I. Baksaas, T. Grande, I. R. Aukrust, and C. A. Drevon, “Bioavailability and Chemical/Functional Aspects of Synthetic MK7 vs Fermentation-Derived MK7 in Randomised Controlled Trials,” International Journal for Vitamin and Nutrition Research, pp. 1–15, Apr. 2016.
- Poundarik, T. Diab, G. E. Sroga, A. Ural, A. L. Boskey, C. M. Gundberg, and D. Vashishth, “Dilatational band formation in bone,” Proceedings of the National Academy of Sciences, vol. 109, no. 47, pp. 19178– 19183, May 2012.
- G. Gast, N. D. Roos, I. Sluijs, M. Bots, J. Beulens, J. Geleijnse, J. Witteman, D. Grobbee, P. Peeters, and Y. V. D. Schouw, “A high menaquinone intake reduces the incidence of coronary heart disease,” Nutrition, Metabolism and Cardiovascular Diseases, vol. 19, no. 7, pp. 504–510, 2009.
- H. J. Choi, J. Yu, H. Choi, J. H. An, S. W. Kim, K. S. Park, H. C. Jang, S. Y. Kim, and C. S. Shin, “Vitamin K2 Supplementation Improves Insulin Sensitivity via Osteocalcin Metabolism: A Placebo-Controlled Trial,” Diabetes Care, vol. 34, no. 9, 2011.
- D. K. Cundiff and P. S. Agutter, “Cardiovascular Disease Death Before Age 65 in 168 Countries Correlated Statistically with Biometrics, Socioeconomic Status, Tobacco, Gender, Exercise, Macronutrients, and Vitamin K,” Cureus, 2016. BK. McFarlin, et al. “Oral Consumption of Vitamin K2 for 8 Weeks Associated With Increased Maxmal Cardiac Output During Exercise.” Altern Ther Health Med. 2017 vol. 23, no. 4, pp.26-32. 2017.Feb;59(2):186-95.
- F. Oury, L. Khrimian, C. A. Denny, A. Gardin, A. Chamouni, N. Goeden, Y.-Y. Huang, H. Lee, P. rinivas, X.-B. Gao, S. Suyama, T. Langer, J. J. Mann, T. L. Horvath, A. Bonnin, and G. Karsenty, “Maternal and Offspring Pools of Osteocalcin Influence Brain Development and Functions,” Cell, vol. 155, no. 1, pp. 228–241, 2013.
- Y. Gat, M. Gornish, M. Heiblum, and S. Joshua, “Reversal of benign prostate hyperplasia by selective occlusion of impaired venous drainage in the male reproductive system: novel mechanism, new treatment,” Andrologia, vol. 40, no. 5, pp. 273–281, 2008.
- Cario-Toumaniantz, C. Boularan, L. J. Schurgers, M.-F. Heymann, M. L. Cunff, J. Léger, G. Loirand, and P. Pacaud, “Identification of Differentially Expressed Genes in Human Varicose Veins: Involvement of Matrix Gla Protein in Extracellular Matrix Remodeling,” Journal of Vascular Research, vol. 44, no. 6, pp. 444–459, 2007.
- Turck, et al. “Dietary Reference Values for vitamin K.” EFSA Journal, vol. 15, no.6 pp 4780, 2017.
- Riphagen, et al. “Prevalence and Effects of Functional Vitamin K Insufficiency: The PREVEND Study.” Nutrients, vol. 9, no. 12, p. 1334. Aug 2017.
- Brown. “Canadian Data Provide Window on Statin Use.” Canadian Medical Association Journal, vol. 188, no. 5, 2016, pp. 325–325.
- Theuwissen, et al. “Vitamin K Status in Healthy Volunteers.” Food Funct., vol. 5, no. 2, 2014, pp. 229–234.
- H. Okuyama, P. H. Langsjoen, N. Ohara, Y. Hashimoto, T. Hamazaki, S. Yoshida, T. Kobayashi, and A. M. Langsjoen, “Medicines and Vegetable Oils as Hidden Causes of Cardiovascular Disease and Diabetes,” Pharmacology, vol. 98, no. 3-4, pp. 134–170, 2016.
- M. K. Shea, C. J. Odonnell, C. Vermeer, E. J. P. Magdeleyns, M. D. Crosier, C. M. Gundberg, J. M. Ordovas, S. B. Kritchevsky, and S. L. Booth, “Circulating Uncarboxylated Matrix Gla Protein Is Associated with Vitamin K Nutritional Status, but Not Coronary Artery Calcium, in Older Adults,” The Journal of Nutrition, vol. 141, no. 8, pp. 1529–1534, 2011.
- S. Lamon-Fava. “Statins and Lipid Metabolism.” Current Opinion in Lipidology, vol. 24, no. 3, pp. 221–226, 2013.
- M. J. Shearer, X. Fu, and S. L. Booth, “Vitamin K Nutrition, Metabolism, and Requirements: Current Concepts and Future Research,” Advances in Nutrition, vol. 3, no. 2, pp. 182–195, Jan. 2012.
- P. Newman and M. J. Shearer, “Metabolism and cell biology of vitamin K,” Thrombosis and Haemostasis, vol. 100, no. 10, pp. 530–547, 2008.
- L. J. Schurgers and C. Vermeer, “Differential lipoprotein transport pathways of K-vitamins in healthy subjects,” Biochimica et Biophysica Acta (BBA) – General Subjects, vol. 1570, no. 1, pp. 27–32, 2002.
- T. Sato, L. J. Schurgers, and K. Uenishi, “Comparison of menaquinone-4 and menaquinone-7 bioavailability in healthy women,” Nutrition Journal, vol. 11, no. 1, Dec. 2012.
- T. Dayspring, “Postprandial and Fasting Lipids,” http://www.lipidcenter.com/pdf/Postprandial_and_Fasting_Lipids.pdf.2018.
- P. Newman, F. Bonello, A. S. Wierzbicki, P. Lumb, G. F.Savidge, and M. J. Shearer, “The Uptake of Lipoprotein- Borne Phylloquinone (Vitamin K1) by Osteoblasts and Osteoblast-Like Cells: Role of Heparan Sulfate Proteoglycans and Apolipoprotein E,” Journal of Bone and Mineral Research, vol. 17, no. 3, pp. 426–433, Jan. 2002.
- H. Okuyama, P. H. Langsjoen, T. Hamazaki, Y. Ogushi, R. Hama, T. Kobayashi, and H. Uchino, “Statins stimulate atherosclerosis and heart failure: pharmacological mechanisms,” Expert Review of Clinical Pharmacology, vol. 8, no. 2, pp. 189–199, Jun. 2015.
- Takeuchi et al., “Minimal effective dose of vitamin K2 (Menaquinone-4) on serum osteocalcin concentration in Japanese subjects and safety evaluation of vitamin K2 supplemented in calcium tablet,” Journal of Japan Society of Nutrition and Food Sciences, vol. 26, pp. 254–260, 2005.
- N. Inaba, T. Sato, and T. Yamashita, “Low-Dose Daily Intake of Vitamin K2 (Menaquinone-7) Improves Osteocalcin γ-Carboxylation: A Double- Blind, Randomized Controlled Trials,” Journal of Nutritional Science and Vitaminology, vol. 61, no. 6, pp. 471–480, 2015.
- L. J. Schurgers, K. J. F. Teunissen, K. Hamulyak, M. H. J. Knapen, H. Vik, and C. Vermeer, “Vitamin K-containing dietary supplements: comparison of synthetic vitamin K1 and natto-derived menaquinone-7,” Blood, vol. 109, no. 8, pp. 3279–3283, 2007.
- M. H. J. Knapen, L. J. Schurgers, and C. Vermeer, “Vitamin K2 supplementation improves hip bone geometry and bone strength indices in postmenopausal women,” Osteoporosis International, vol. 18, no. 7, pp. 963–972, Aug. 2007.